Practical Guidance for Selecting Key Performance Indicators in Healthcare

Introduction
Key Performance Indicators in healthcare as defined by HIQA (2012) are specific and measurable elements of practice that can be used to assess quality and safety of care. A Key Performance Indicator (KPI) differs from an audit as the KPI is an indicator of areas that require further follow up and investigation, where an audit is an assessment of performance against a set of standards or criteria in a health or social care service.
In this blog, we look at the purpose of healthcare KPIs and offer guidance on selecting what KPIs to monitor for your service and suggest what parameters should be considered for monitoring the data.
What is the purpose of Key Performance Indicators in Healthcare
The purpose of healthcare KPIs include:
- Indication of what is going on.
- Help to keep an eye on the core areas of the service and how they are performing.
- Indicates areas that require further follow up.
- Beneficial for both Senior Management and Department Heads.
Practical Suggestions for Selecting Healthcare KPIs
When selecting healthcare KPIs, HIQA (2013) suggest considering the following when choosing areas to measure:
- Importance of the problem
- Service-user safety
- Potential for improvement
- Controllability by health or social care system/professionals
- Consider measures across multiple domains.
Below are some further practical considerations for setting KPIs:
- Consider the applicable Standards / Regulations to identify relevant headings that can be used to build a framework of KPIs, e.g. HIQA Themes.
- Identify KPIs related to both direct care and non-direct care (e.g. governance, supplies, fire safety, staff fire training etc).
- Consider the areas core to the service being provided (e.g. in medical transport service, response times).
- Consider areas of high risk (e.g. in screening service, the management of diagnostic results).
- Consider areas that have recently been of concern – e.g. complaints, audit findings, incident reports, etc.
- Consider areas where there is data which can realistically be gathered.
- Consider under the headings of Structure, Process and Outcome.
Examples of KPIs
- Number of Falls
- Number of Falls with Injury
- Number of Complaints
- Number of Incidents
- Number of Medication Errors
- Number of High Risk Medication Errors
- % of Residents who have received Flu Vaccination
- % Turnover of Staff
- Number of Management Meeting held as per schedule
- Number of QIPs closed as per schedule
Setting the Parameters for each KPI
When developing healthcare KPIs, it is important to ensure they are clearly defined, and have all relative parameters, including but not limited to:
- KPI Title: Include the exact title of the KPI, for example “Number of Falls”.
- KPI Description: Provide a description of the KPI including a description of the target population.
- KPI Rationale: Outline the reason for measuring this KPI.
- KPI Target (if appropriate): Indicate the target for the KPI, for example “Ongoing improvement”.
- KPI Calculation – Numerator and denominator: Outline how the KPI shall be calculated, either whole number or %.
- Data Source: Detail the source of the required data, for example incident reports which report a fall.
- Collating Frequency: Specify how often data is to be collected and reported. Shall it be daily / weekly / monthly / quarterly / bi-annually / annually)
- Responsibility for Collecting Data: Detail the person responsible for gathering the data.
- Report to: Detail the person or group the data is reported to, who has responsibility for analysing and interrogating the data. For example the Senior Management Team.
Presentation and Analysis of Healthcare KPI data
KPI data must be displayed in a graph so that you can view the trend over time. When preparing the graph, it is important to include the time period and the numerical / percentage measure. See example below.
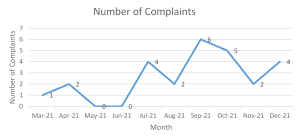
When analysing and interrogating the data, ensure this is completed by the relevant individuals or groups on a regular basis. Ensure sufficient time is allocated and that consideration is given to the changes in the data, the trends in data and any unusual results.
Actions identified from the analysis should be managed as per the Quality Improvement Plan (QIP) process. Audit may be reviewed to determine the root cause of the results.
How can HCI help?
At HCI, we help providers of health and social care make intelligence driven decisions to attain, manage and improve quality, safety and regulatory compliance. We work with clients to help them define the appropriate Key Performance Indicators that will support them in measuring the success of their service and provide relevant data to demonstrate regulatory compliance or support the achievement of JCI accreditation or CHKS accreditation. We can also analyse and trend the KPI data on a monthly or quarterly basis and provide an independent and objective opinion as to where improvements need to be made. This will save you time in analysing your data and developing action plans.
Click here to find out more about our Quality and Safety Data Analysis Service.
For more information contact HCI at 01 629 2559 or info@hci.care.
References
HIQA (2012). National Standards for Safer Better Healthcare, 2012. Dublin: Health Information and Quality Authority.
HIQA (2013). Guidance on Developing Key Performance Indicators and Minimum Data Sets to Monitor Healthcare Quality, 2013. Dublin: Health Information and Quality Authority.